Industry Growth
The medical billing industry has been steadily growing over the last five years. According to IBIS World, the industry has seen an average of 3.1% growth to $4.3 billion from 2015-2020. While many sources have said that the industry has taken a small hit in 2020 due to the Covid-19 pandemic, the industry is expected to quickly rebound. The market is projected to hit $12.44 billion by 2023 at an annualized growth rate of 13.93%.
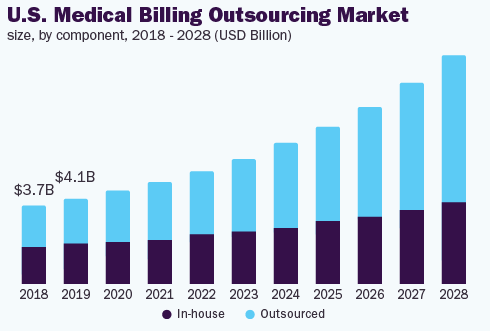
As you can see by the Grandview Research chart above, the outsourced medical billing market is expected to keep growing. Some influencing factors include new technological solutions offered by providers, increasing government requirements and updates, and a rising percentage of denied claims. These numbers are promising and present a good opportunity for outsourced medical billing companies over the next several years.
Market Share
When it comes to outsourced medical billing, hospitals make up the largest source of revenue as of 2020. This is because they typically have the largest volume of claims. Additionally, hospitals typically face the largest variety and complexity of claim types, leading them to outsourcing solutions. The chart below shows the market share as of 2019, but it also holds true for 2020.
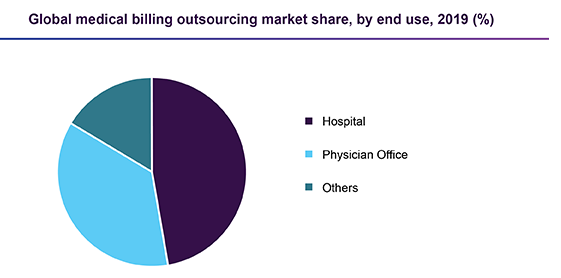
The second largest source of revenue in the medical billing industry is physicians offices. According to Grandview Research, physicians offices are likely to expand at the fastest rate over the next several years. This is partly due to the rising number of services they provide as well as billing and coding updates.
Influencing Factors
Need to Simplify Claims Process
More and more medical practices every year are looking for ways to simplify their claims process, reduce billing errors, and maximize their revenue. According to MarketWatch,
“Unless an office or a medical practice is using services of an experienced billing provider who has been trained to look at holes in paperwork, there’s a good chance that their revenue is not as high as it could be.”
Market Watch
There is a growing focus on risk management in the medical industry, and more practices are seeing the value that outsourced medical billing providers bring to the table – in terms of efficiency, accuracy, and cost-time benefits.
Digital Record-Keeping and Automation
Medical practices today are almost entirely digital in terms of record-keeping and practice management. As of 1996, practices have to keep digital records (EMR) of their patients health charts. In addition, there is other cloud-based software that practices have adopted to keep more secure records and efficiently manage their practice. Due to the number of cloud-based platforms practices must now manage, many are seeing the value in working with an outsourced billing provider. Outsourced providers often offer all-in-one, streamlined software options that practices can easily navigate on the back-end.
High technology costs
Medical billing software and in-house administration are becoming more expensive every year. When medical practices do not use an outsourced medical billing provider, they incur several overhead costs. These costs include software, EMR databases, administrative salaries and benefits, and much more. Using an outsourced medical biller typically saves practices money on software, billing, and administrative costs, leading more practices to switch to outsourcing year over year.
COVID-19 Impact
Although the industry has grown steadily this year, Covid-19 has certainly impacted the medical billing industry in certain ways.
Lower Health Insurance Coverage
Unfortunately, since Covid-19 hit the U.S., there has been a sharp increase in unemployment across the country. As a result, less people across the country are able to obtain health insurance coverage this year. This has impacted the medical billing industry by preventing many Americans from visiting healthcare centers without private insurance. However, as the economy rebounds and more Americans return to work, this trend is likely to taper off.
New Tracking and Coding Updates
The government has released new codes that billing and coding professionals must use to diagnose and treat Covid-19. There are various codes for different Covid-related procedures, such as testing, diagnoses, patient exposure, etc. what is more, the CDC continues to update these codes as they learn new information about Covid-19. These complications may be leading to more medical practices outsourcing their billing needs so they can focus on operations.
Need to Reduce Denied Claims
Due to the struggling economy and lower patient volume, many healthcare practices are finding new incentive to lower denied claims rates. Each denied claim costs practices money to correct. So in order to maximize their revenue, many practices are seeking help from third-party medical billers to keep denied claim rates down.
Patient Volume and Telehealth
Some healthcare facilities, such as hospitals, are seeing a rise in patient volume due to Covid-19. Others still are switching over to telehealth or remote care options. These factors alone are causing such types of medical practices to opt for outsourced medical billing solutions, to either free up time for patient care or facilitate remote operations.
North America Market
North America has held the highest market share when it comes to outsourced medical billing. One reason for this is that U.S. healthcare providers are looking for tech-savvy, end-to-end solutions for managing their practice’s revenue. Many practices need a solution for efficiently managing the high volume of Medicare and Medicaid claims. There is also an increased awareness in the U.S. when it comes to the solutions and benefits offered by third-party, outsourced medical billing providers. Additionally, ICD-10 codes in the U.S. are among the most complicated worldwide, leading many practices to opt for the simplicity of revenue cycle management services (RCM).
U.S. Competition and Industry Leaders
Competition in the outsourced medical billing industry is considered fairly competitive and fragmented, since many small and mid-size providers must compete with one another. This combined with the fact that demand for medical billing services is increasing is fostering competition. However, market share concentration among industry leaders is fairly low, as the largest players make up a small share of the market relatively. Among the top players in the outsourced medical billing industry include:
- HMS Holdings Corp.
- Cerner
- McKesson Corp.
- EClinicalWorks
- GE Healthcare
- Allscripts Healthcare Solutions
- Kareo
- Quest Diagnostics
- AthenaHealth
Small medical billing providers can offer streamlined medical billing solutions and focus on their cost to remain competitive.
Further Reading
360Connect has additional resources for those in the medical billing space. Learn more about starting your own medical billing company, or learn how to get more medical billing clients. Also check out our Supplier program – we help medical billing providers find new customers and grow their revenue.
